Abstract
Background: Chronic granulomatous disease (CGD) is a congenital immunodeficiency characterized by severe life-threatening infections. CGD patients lack reactive oxygen species (ROS) in phagocytic leukocytes and often develop widespread tissue granulomas. The current treatment for CGD is lifelong antibiotic prophylaxis or hematopoietic stem cell transplantation (HSCT). However, most patients cannot find matched donors, and HSCT is known to have increased risk in CGD patients. Gene therapy has become a promising treatment for CGD. At present, "ex vivo" HSC gene therapy is the widely applied strategy. "In vivo" gene therapy is based on direct delivery of gene therapy vectors into patients, which could overcome the difficulties in HSCT.
Methods: We have developed an in vivo CGD gene therapy strategy by intravenous (iv) injection of lentiviral vectors (LVs) carrying an universal EF1a promoter or a myeloid-specific miR223 promoter driving the expression of CYBB (cytochrome B-245 beta chain, or p91-phox) in X-CGD mice (X-CGD; B6.129S-Cybbtm1Din/J). Each mouse received 1x109 transduction units (TU) of LV-CYBB via iv injection after non-myeloablative conditioning. A second injection of 1x109 TU of LV-CYBB after re-conditioning was given 12 weeks later.
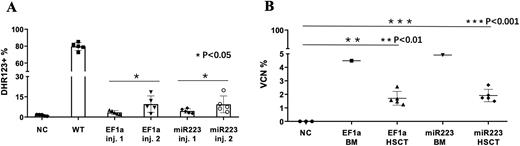
Results: We developed a chemotherapy conditioning regimen to improve gene delivery efficiency by using busulfan, cyclophosphamide and dexamethasone. The X-CGD mice received two iv injections of LVs, and the expression and function of the LV-CYBB gene were analyzed by intracellular gp91-phox staining and DHR123 assay 4 weeks after each injection. Based on flow cytometry, we detected gp91-phox positive cells in the blood as the following, EF1a: 1.14-5.18% and 5.27-14.36%, and miR223: 1.65-5.17% and 4.59-17.89% after the first and the second injections, respectively, as compared with the WT mice: 79.9-87.6%. Functional analyses of ROS showed the following, EF1a: 1.93-5.2% and 2.39-18.51%, miR223: 2.65-6.67% and 3.75-19.8%, after the first and the second injections respectively, as compared with WT: 72.6-85.31% (Figure A). The LV vector copy number (VCN) in the peripheral blood mononuclear cells was detected by qPCR as the following, EF1a: 1.11-2.32% and 1.35-9.32%, and miR223: 1.01-2.39% and 2.71-8.51% after the first and the second injections, respectively. These results indicated that iv LV injection effectively delivered and expressed the LV-CYBB gene in vivo, and repeated injection of the LVs could increase the gene transfer efficiency in the CGD mice. Importantly, after the second injection, we found no antibody response to the LV particle-associated protein p24. However, after 3-12 months, markedly reduced VCN was found in the blood of the treated mice, suggesting exhaustion of the transgenes in the somatic cells. To improve the gene delivery into HSCs, we treated the mice with AMD3100 to mobilize HSCs into peripheral blood. The mice were treated with chemo-conditioning and AMD3100 prior to LV ivinjection. After four weeks, the gp91-phox positive HSCs of total Sca1+ HSCs in blood with or without (+/-) AMD3100 treatment were examined by flow cytometry, and the results showed the following, EF1a: (-) 9.52-15.43%, (+) 16.1-29.4%, and miR223: (-) 4.49-10.35% and (+) 7.06-16.84%. To confirm stem cell gene transfer, we transplanted the bone marrow cells from the LV-CYBB-treated CGD mice into untreated CGD mice. The VCN in blood was examined before (donor mice) and 4 weeks after (recipient mice) the HSCT, and the results showed the following, EF1a: before 4.49% (in the donor) and after 1.05-2.57% (in the recipients), and miR223: before 4.91% (in the donor) and after 1.04-2.69% (in the recipients) (Figure B). This transplantation study confirmed that the AMD3100 treatment effectively increased iv LV gene delivery into HSCs.
Conclusion: We have developed an improved LV iv gene delivery strategy by applying chemo-conditioning and AMD3100 mobilization prior to the injection of the LVs into CGD mice. This in vivo LV gene therapy strategy could potentially be translated into future CGD gene therapy applications.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal